It might be possible for human-to-human airborne transmissible avian H5N1 influenza viruses to evolve in nature, new research has found.
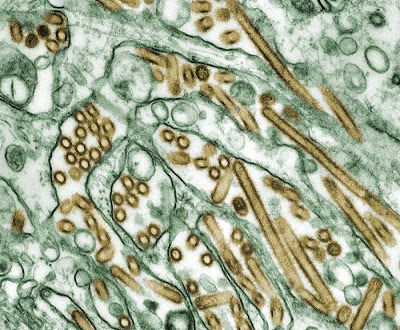 |
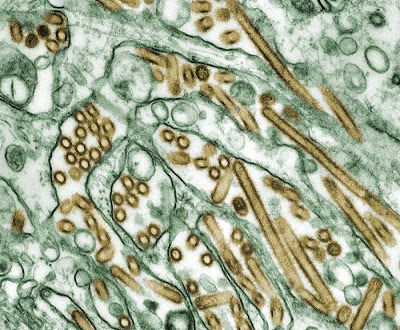
| Colorized transmission electron micrograph of Avian influenza A H5N1 viruses (seen in gold) grown in MDCK cells (seen in green) [Credit: CDC/Courtesy of Cynthia Goldsmith; Jacqueline Katz; Sherif R. Zaki] |
The findings, from research led by Professor Derek Smith and Dr Colin Russell at the University of Cambridge, were
published June 22 in the journal Science.
Currently, avian H5N1 influenza, also known as bird flu, can be transmitted from birds to humans, but not (or only very rarely) from human to human. However, two recent papers by Herfst, Fouchier and colleagues in Science and Imai, Kawaoka and colleagues in Nature reveal that potentially with as few as five mutations (amino acid substitutions), or four mutations plus reassortment, avian H5N1 can become airborne transmissible between mammals, and thus potentially among humans. However, until now, it was not known whether these mutations might evolve in nature.
The Cambridge researchers first analysed all of the surveillance data available on avian H5N1 influenza viruses from the last 15 years, focusing on birds and humans. They discovered that two of the five mutations seen in the experimental viruses (from the Fouchier and Kawaoka labs) had occurred in numerous existing avian flu strains. Additionally, they found that a number of the viruses had both of the mutations.
Colin Russell, Royal Society University Research Fellow at the University of Cambridge, said: "Viruses that have two of these mutations are already common in birds, meaning that there are viruses that might have to acquire only three additional mutations in a human to become airborne transmissible. The next key question is 'is three a lot, or a little?' "
The scientists explored this key question using a mathematical model of how viruses replicate and evolve within a mammalian host and assessed the influence of various factors on whether the remaining three mutations could evolve in a single host or in a short chain of transmission between hosts
The factors that increased the likelihood of mutations evolving are:
1. Random mutation. The replication mechanisms of influenza viruses don't make perfect copies. On average, every time an influenza virus replicates itself it makes approximately one mutation somewhere in the genome of each new virus. In each infected human there will be billions of viruses, and thus with many viruses replicating, multiple mutations can accumulate within a single host.
2. Positive selection. If some of the remaining mutations help the avian virus to adapt to mammals, then those mutations will make the viruses more fit and thus will be positively selected and preferentially accumulate.
3. Long infection. The longer someone is infected and producing new viruses, the more time there is for mutations to accumulate.
4. Functionally equivalent substitutions. The sets of substitutions identified by Fouchier and Kawaoka are unlikely to be the only combinations of substitutions capable of producing an aerosol transmissible virus. The probability of emergence increases with the number of combinations.
5. Diversity in the within-bird virus population. Given all of the mutations there are likely to be within a host due to random mutation, it is possible that the viruses from a bird that infect a human might have a mutation that would not be detected by routine surveillance. For example, if 100 virus particles from a bird infect a human and one of those particles had a key mutation, it would increase the probability of the mutation reaching high levels within a host even though routine sequencing would not detect it.
6. Transmission between mammals. If mammals are capable of transmitting viruses that have some but not all of the necessary substitutions it could increase the probability of an airborne transmissible virus evolving.
The factors that decreased the likelihood of mutations evolving are:
1. An effective immune response. An effective immune response would shorten the length of an infection and thus decrease the time available to accumulate mutations.
2. Deleterious substitutions. If any of the substitutions necessary for airborne transmission were harmful to the virus it would, on average, slow the accumulation of mutations.
3. Order of acquiring mutations. It is not currently known if the mutations for airborne transmissibility need to be acquired in a specific order. If they do, it would, on average, slow the accumulation of mutations.
"With the information we have, it is impossible to say what the exact risk is of the virus becoming airborne transmissible among humans. However, the results suggest that the remaining three mutations could evolve in a single human host, making a virus evolving in nature a potentially serious threat," said Derek Smith, Professor of Infectious Disease Informatics at the University of Cambridge. "We now know that it is in the realm of possibility that these viruses can evolve in nature, and what needs to be done to assess the risk more accurately of these mutations evolving in nature."
The scientists recommend the following activities be considered high priority for estimating and ameliorating the risk of emergence of aerosol transmissible H5N1 viruses.
First, additional surveillance in regions where viruses with airborne transmission enabling substitutions have been observed and in regions connected to those regions by bird migration and trade. Also, increased surveillance for mutations that might have the same function as those found by the Fouchier and Kawaoka labs.
Second, related to surveillance, some targeted sequencing of H5N1 viruses should be done by "deep sequencing" where the lab sequences many viruses from an individual host to look for viruses that might have accumulated the critical mutations, even if those viruses are just a small proportion of the viruses within an animal.
Third, further investigations are needed to determine which substitutions and combinations of substitutions that are not the same as, but have the same function as, the substitutions identified by the Fouchier and Kawaoka labs are capable of making viruses airborne transmissible between mammals.
Fourth, further studies are needed to elucidate the changes in within-host fitness and between-host transmissibility associated with each airborne transmission enabling substitution and combination of substitutions.
Professor Smith added: "The situation is similar to assessing the risk of an earthquake or tsunami. We don't know exactly when and where, but by increasing monitoring and research -- some of which is already underway -- scientists and public health officials will be able to increase the accuracy with which the risk can be assessed and to minimise those risks."
The research was funded by multiple sources including the European Commission through framework 7 grants EMPERIE and ANTIGONE, the Royal Society, the Human Frontiers Science Program, the Wellcome Trust, and the National Institutes of Health.
Source: University of Cambridge [June 21, 2012]